
Break The Cycle Of Pain

Consultation
Our counseling approach has been designed to assist you with tapping into your full potential throughout your pain management experience. We will provide you with the added insight you need to set personal or professional goals, which will give you the life you really want.

Compliance
We can assist you throughout your pain management experience with adhering to your doctor’s recommended course of treatment. We understand that there are many factors that lead to non-compliance; several of which, can be unforeseen and out of your control. However, most of the factors that lead to non-compliance can be changed with little effort.

Community
We provide workshops aimed to foster a sense of community and provide valuable support for individuals grappling with chronic pain by creating a space for shared experiences and collaborative strategies.
Helping you take control of your chronic pain
Pain is an all-too-familiar problem and the most common reason that people see a physician. Unfortunately, alleviating pain isn't always straightforward.
At least 100 million adults in the United States suffer from chronic pain, according to the Institute of Medicine. The American Academy of Pain Medicine reports that chronic pain affects more Americans than diabetes, heart disease and cancer combined.
Understanding and managing the thoughts, emotions and behaviors that accompany your discomfort can help you cope more effectively with your pain — and can actually reduce the intensity of your pain.
Read Our Latest Blogs

Reversing the Forces Behind Persistent Pain
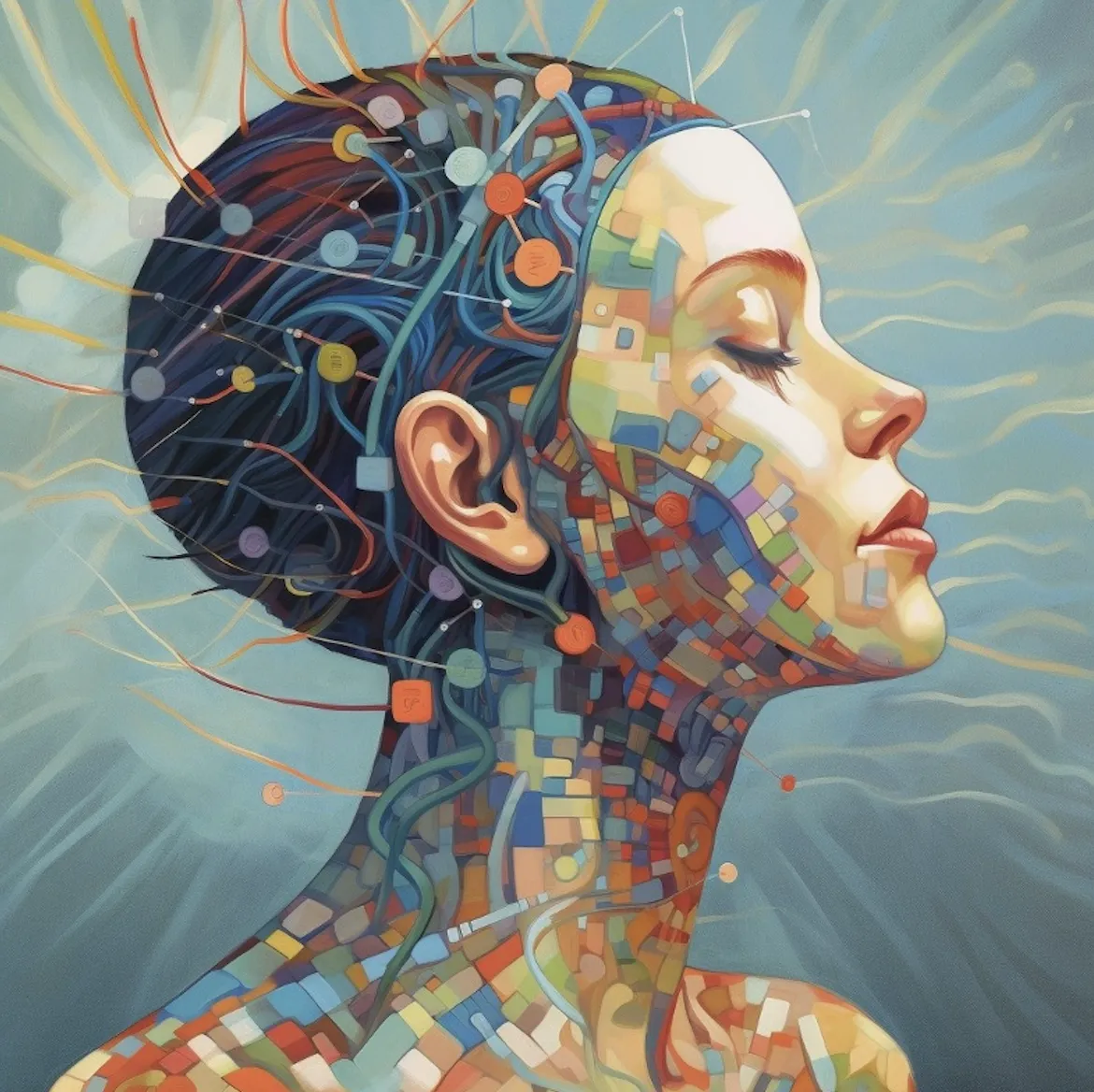
Power of Neuroplastic Transformation: Reversing the Forces Behind Persistent Pain
Introduction
For far too long, the approach to treating persistent pain has focused solely on managing symptoms, attempting to rein in the relentless waves of discomfort. However, a paradigm shift is underway—a shift from symptom management to addressing the root causes that perpetuate pain's persistence. In this blog post, we'll explore the transformative power of neuroplastic transformation in reversing the forces behind persistent pain and restoring normalcy.
Understanding the Forces Behind Persistent Pain
Persistent pain is not a random occurrence but rather a complex interplay of forces within the brain and body that maintain its grip. These forces, ranging from molecular and cellular changes to physiological adaptations, perpetuate the cycle of suffering and hinder the body's ability to return to a state of equilibrium (Vaso et al., 2014).
The Stages of Treatment
Traditional approaches to pain management often fall short in addressing the underlying mechanisms driving persistent pain. However, a new approach is emerging—one that aims to reverse the fundamental forces that maintain pain's persistence. This involves harnessing the incredible power of the brain to:
(1) disconnect expanded pain networks,
(2) halt perpetually firing pain-dedicated nerves,
(3) resolve inflammatory processes,
(4) reverse the energy used to maintain pain receptors, and
(5) restore normal pain responses (Flor & Diers, 2013).
Harnessing Neuroplastic Transformation
At the heart of this transformative approach lies neuroplastic transformation—the brain's remarkable ability to adapt, rewire, and heal. By tapping into this innate capacity for change, individuals can break free from the shackles of persistent pain and reclaim their lives. Through targeted interventions that leverage neuroplasticity, individuals can dismantle the neural circuits that sustain pain and pave the way towards lasting relief (Moseley & Flor, 2012).
Conclusion
The goal of treatment for persistent pain is no longer to merely manage symptoms but to reverse the underlying forces that maintain its persistence. By understanding these forces and the stages of treatment, healthcare providers can unleash the power of neuroplastic transformation to restore normalcy and alleviate suffering. Through innovative research, multidisciplinary collaboration, and a deep understanding of neuroplasticity, we can embark on a journey towards a future where persistent pain is no longer an insurmountable obstacle, but rather a challenge to be overcome with resilience and hope.
References
Apkarian, A. V., & Fields, H. L. (2014). Brain mechanisms of chronic pain: clinical implications. Handbook of Clinical Neurology, 131, 35-58.
Davis, K. D. (2016). Neuroplasticity and chronic pain. Pain Management, 6(1), 71-75.
Moseley, G. L. (2012). Reconceptualizing pain according to modern pain science. Physical Therapy Reviews, 17(3), 123-134.
Woolf, C. J. (2011). Central sensitization: Implications for the diagnosis and treatment of pain. Pain, 152(3 Suppl), S2-S15.
"Pain is not in your head, and the solution is not in your body."
-Dr. Howard Schubiner, MD

© 2024 Connected Care
