Read Our Latest Blogs
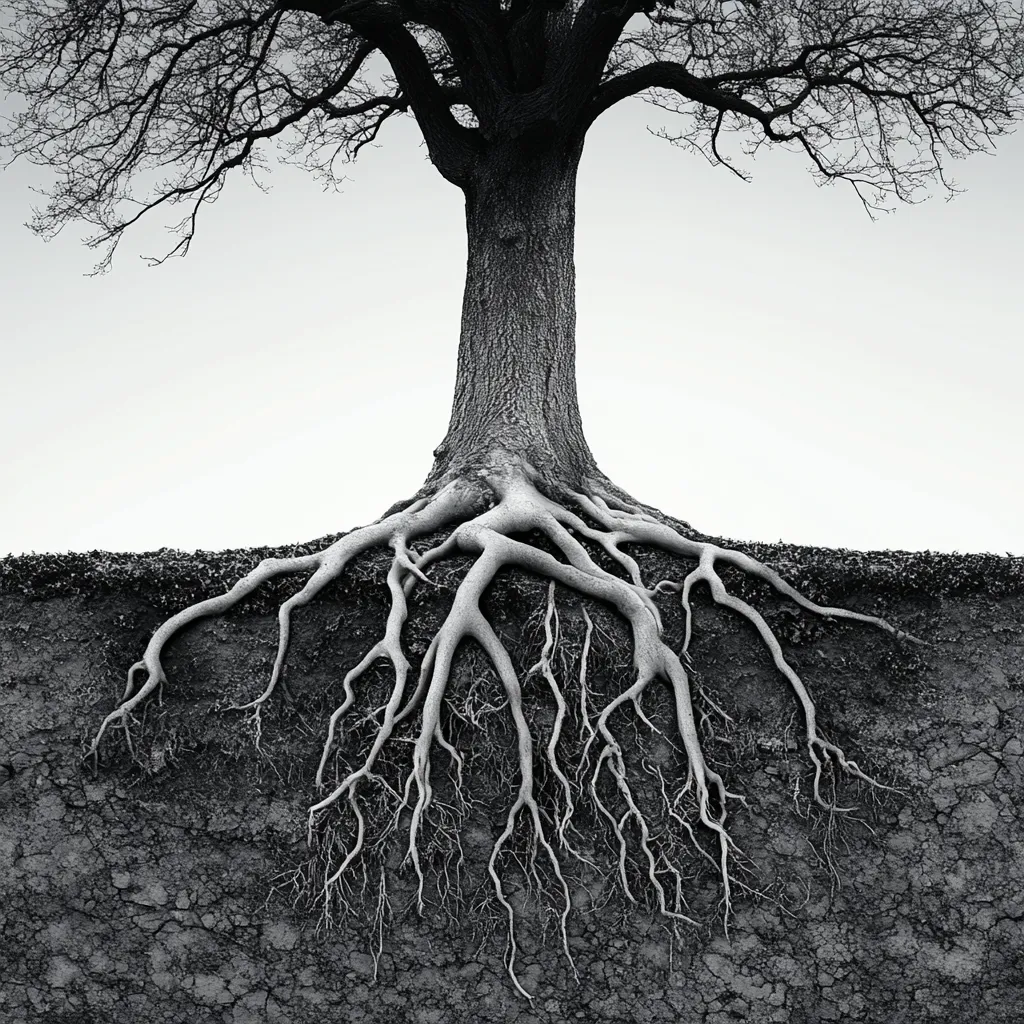
More Than Pain: Uncovering the Hidden Roots of Chronic Pain Suffering
Digging through four of the big public health sites—the American Public Health Association (APHA), the National Partnership for Action to End Health Disparities (NPA), the CDC Health Equity Timeline, and Healthy People 2030—I emerged with reasonable impressions about the interrelationships among social determinants of health (SDOH), chronic disease, and pain management disparities. I feel deeply challenged and inspired to integrate these impressions into my current practice and the future.
A common thread throughout all four portals is the dramatic impact of SDOH, particularly income, education, housing, and access to care, on health outcomes. Healthy People 2030 reports that lower-income populations have much higher rates of preventable chronic diseases—frequently accompanied by chronic pain—such as diabetes, arthritis, and cardiovascular disease (Office of Disease Prevention and Health Promotion [ODPHP], n.d.). Chronic pain in individuals with poverty or those without access to healthy food, nutrition, and healthy environments becomes considerably more difficult to treat. It is an appeal to view beyond symptoms and confront causative forces within our clinical practice.
Equal pain care continues to be out of reach of racial and ethnic minority groups, among whom rates are increased but not care delivery. For example, Black patients are systematically undertreated in emergency care due to implicit biases and outdated assumptions about pain tolerance (National Partnership for Action to End Health Disparities [NPA], n.d.). Similarly, the CDC's Health Equity Timeline explains how decades of structural inequities—such as redlining and continued underfunding of healthcare among marginalized groups—have resulted in current disparities (Centers for Disease Control and Prevention [CDC], 2022).
From APHA, I learned about policy-level interventions and promising community-based solutions for health equity. Behavioral health, combined with culturally responsive care and patient advocacy for pain patients, is being led by increased interventions. These system changes are very much aligned with the trauma-informed care, integrative model that I envision for treating chronic pain—where mental health, physical therapy, and social support are of equal or greater importance than pharmacologic interventions.
References
Centers for Disease Control and Prevention. (2022). Health equity: Timeline of milestones and efforts. https://www.cdc.gov/healthequity/features/timeline/index.html
National Partnership for Action to End Health Disparities. (n.d.). NPA resources. U.S. Department of Health and Human Services, Office of Minority Health. https://www.minorityhealth.hhs.gov/npa
Office of Disease Prevention and Health Promotion. (n.d.). Social determinants of health. Healthy People 2030. https://health.gov/healthypeople/objectives-and-data/social-determinants-health
Complete the form to subscribe to our blog

© 2024 Connected Care
